Malaria, a disease responsible for infecting nearly 250 million people annually and claiming over 600,000 lives, has been a persistent challenge for global health initiatives. While existing vaccines have shown promise, they offer only about 75% effectiveness and require booster doses. In a groundbreaking development, scientists have devised an unconventional vaccination strategy: leveraging genetically modified parasites transmitted through mosquito bites to boost immunity. This novel approach could potentially change the trajectory of malaria eradication efforts.
The Science Behind the Innovation
Malaria is caused by a single-celled parasite, Plasmodium falciparum, transmitted by female Anopheles mosquitoes. Once inside a human host, the parasite travels to the liver, where it multiplies and later invades red blood cells, causing symptoms such as fever, chills, and severe complications like organ failure.
In a recent study published in The New England Journal of Medicine, researchers at the London School of Hygiene and Tropical Medicine explored a unique approach to combat this parasite. They genetically engineered the Plasmodium falciparum parasite to halt its development shortly after infection, allowing the immune system to recognize and develop defenses against the invader. In human trials, nearly 90% of participants exposed to the modified parasites avoided contracting the disease after being bitten by malaria mosquitoes.
A Tale of Two Parasites: GA1 vs. GA2
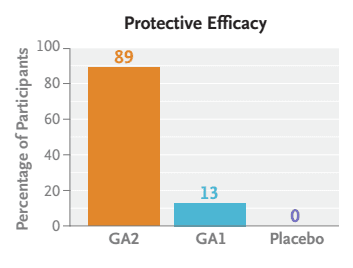
The study tested adults who had not had malaria and were randomly assigned to receive 50 bites from GA2-infected mosquitoes, 50 bites from GA1-infected mosquitoes, or 50 bites from uninfected mosquitoes (placebo), in three immunization sessions at 28-day
intervals.
- GA1 Parasite: Programmed to cease development 24 hours after infection, it showed limited success, protecting only 13% of participants from malaria.
- GA2 Parasite: Halted development six days post-infection, during the parasite’s crucial liver replication phase. This version proved far more effective, with 89% of participants avoiding malaria after exposure to GA2-modified parasites.
Three weeks later, these adults were exposed to malaria-carrying mosquitoes. The results demonstrated significantly higher antibody levels in participants bitten by GA2 mosquitoes, confirming the potential of this strategy.
Julius Hafalla, an immunologist at the London School of Hygiene and Tropical Medicine, remarked, “These findings represent a significant step forward in malaria vaccine development. The ongoing global malaria burden makes the development of more effective vaccines a critical priority.”
Safety and Ethical Considerations
One of the trial’s noteworthy aspects was its safety profile. Despite the unconventional delivery method involving mosquito bites, participants experienced minimal side effects beyond itching. Researchers were careful to ensure that the genetically modified parasites could not progress to the blood stage, effectively eliminating the risk of full-blown malaria.
However, the approach does raise ethical concerns. For instance, would large-scale deployment of genetically modified mosquitoes be socially acceptable? Could releasing such mosquitoes disrupt local ecosystems? These are questions researchers must address in future studies.
A Vision for the Future
If larger trials confirm GA2’s effectiveness, this strategy could open new doors for malaria control. Hypothetically, swarms of GA2-infected mosquitoes could serve as mobile vaccination units in malaria-endemic regions, delivering immunity during high-risk seasons. This approach would bypass the logistical challenges of traditional vaccines, such as cold storage, sterile equipment, and trained healthcare workers.
That said, practical challenges remain. Culturing GA2 parasites involves growing them on human blood cells in a lab before feeding them to mosquitoes. This process is labor-intensive, time-consuming, and expensive. Moreover, continually breeding modified mosquitoes to outnumber wild ones would be a monumental task, both scientifically and administratively.
Beyond Malaria: Broader Implications
While this strategy shows promise for malaria, it may not be easily adaptable to other diseases. The unique lifecycle of Plasmodium falciparum allows it to act as both a vaccine and a vector, a characteristic not shared by many pathogens. Still, the success of this study underscores the importance of innovation in vaccine development, especially for diseases with limited existing solutions.
The Road Ahead
The researchers are eager to replicate their results in larger trials, bringing the world closer to a new era of malaria control. However, they caution that more studies are needed to confirm GA2’s viability as a candidate for global malaria eradication efforts.
The fight against malaria is far from over, but breakthroughs like this offer hope for a future where the disease no longer claims lives. For now, the study serves as a testament to human ingenuity in tackling one of the world’s deadliest parasites.